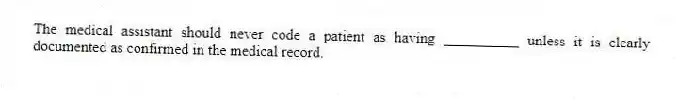
The medical assistant should never code a patient as having __________ unless it is clearly documented as confirmed in the medical record.
Correct Answer:
Verified
The medical assistant shou...
View Answer
Unlock this answer now
Get Access to more Verified Answers free of charge
Q22: The _ table describes malignancies.
Q23: The codes for pernicious anemia and a
Q24: The coder should always refer to the
Q25: Main terms appear in bold type.
Q26: Burns are coded to the site by
Q27: Carcinoma _ is defined as the absence
Q29: Etiology refers to the underlying cause or
Q30: A neoplasm or new growth is coded
Q31: The "code first" notation can usually be
Q32: At times, the medical assistant must code
Unlock this Answer For Free Now!
View this answer and more for free by performing one of the following actions

Scan the QR code to install the App and get 2 free unlocks

Unlock quizzes for free by uploading documents